Last Updated March 2023
What is melasma?
Melasma is a form of skin pigmentation that is stimulated by several factors, with the most notable being oestrogen; either from pregnancy, the pill, hormone replacement therapy or simply naturally occurring higher levels of oestrogen. As a result, melasma mostly affects women, especially between the ages of 20 and 40, although it can occur uncommonly in men.
When melasma begins to develop, it may appear in symmetrical brown patches. It is usually located on the cheeks, upper lip, brows, or forehead, but some cases can result in brown pigmentation developing on the neck, chest or arms.
Most people who are affected by melasma tend to have a more olive or dark skin tone. Additionally, while hormone factors are the main cause of melasma, prolonged sun exposure can also result in the spread of pigmentation. Anyone can develop melasma and while it poses no serious health risks, it can be treated early on to minimise its appearance.

What causes melasma?
The cause of melasma is not clear, but may be due to hormonal changes occurring in the body. Some factors that may influence the production of melasma include the following.
Gender
Women more commonly experience significant hormonal changes than men, particularly as they undergo pregnancy or utilise the contraceptive pill to control their ovulating cycles. Due to these changes, as well as other milestones like menopause, women are more likely than men to develop melasma.
Hormones
The hormonal factors that women experience more than men include higher levels of oestrogen and progesterone. When individuals experience a stronger influence of these hormones, it is highly likely to develop melasma in their skin.
Hormonal influences that may cause melasma include:
- Pregnancy
- Menopausal hormone therapy
- Dosage of an oral contraceptive pill containing oestrogen and progesterone
- Intrauterine implants and devices
The development of skin pigmentation is so common during pregnancy that people often refer to the skin condition as the ‘mark of pregnancy’. However, it is possible that you may not even develop melasma while pregnant.
Genetics
It is a working theory that melasma is a genetic skin condition, namely because roughly 60% of patients with melasma have a positive family history. There is no conclusive evidence as of yet.
Skin type
Due to melanin production being stimulated by UV rays, it has been noted that long-lasting hyperpigmentation is likely to be more evident in the darker skin tones that absorb it better.
Sun exposure
UV radiation may be a key factor in the formulation of melasma, and as such, those affected with melasma often first notice it appears during or after a summer when they have had significant UV exposure.
The blue light from the sun’s visible rays is the main aggravating factor, which can be protected against with appropriate care and sun avoidance.
Heat exposure
There is a belief that melasma can also occur through extended occupational heat exposure, or by being close to cooking fires, which causes UV light and thermal damage. Waxing can also lead to worsening of melasma, so avoid waxing areas affected by melasma.
Medications
Some ingredients found in cosmetic products or even perfumed soaps may cause a phototoxic reaction, leading to the onset of melasma.
These include:
- Antimalarial products
- Anti-epileptic products
- Antipsychotics
- Cytotoxic/Antineoplastic products
It is important to try to determine if any causative factors in your skincare products or medications may be exacerbating the pigmentation.
What are the different types of melasma?
Before melasma can be treated, it is important to know what kind it is. This is because the different types of melasma have separate characteristics, especially in how melanin cells are developed, and may require alternate treatment methods. The types are usually determined by using a specialised light called a wood’s lamp.
Epidermal
Epidermal melasma refers to excess melanin being displayed in the outermost (epidermal) layers of the skin. It is further characterised by a strong, well-defined border, dark brown pigmentation, and a fairly good response to treatment.
Dermal
The middle layer of the skin is where dermal melasma occurs, which displays itself in blue, grey or brown pigmentation. The borders are less clearly defined than epidermal melasma, and the skin condition is harder to treat.
Mixed
The combination of epidermal and dermal melasma results in mixed melasma, whose pigmentation is brown-grey and can be difficult to treat.
Where is melasma most common?
Each case of melasma pigmentation has its own type of distinct patterns and common manifestation sites on the body. The areas melasma is most common are:
- Centrofacial – Accounting for 50-80% of presentations and can be found on the cheeks, forehead, nose and upper lip (bar the philtrum)
- Malar – Cheeks and nose
- Mandibular – Jawline and chin
- Extra facial – Shoulders, upper arms and forearms, following the most sun-exposed areas
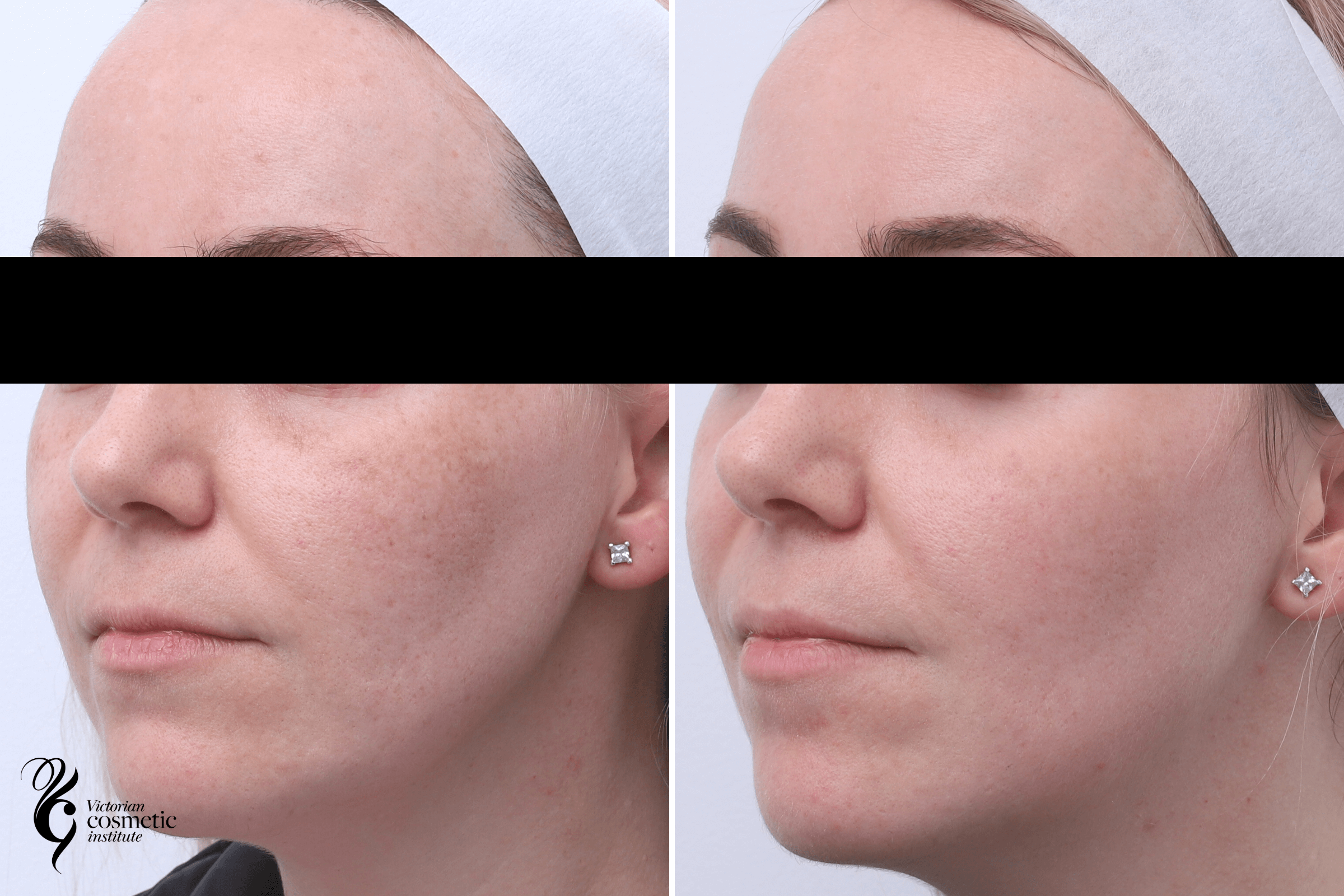
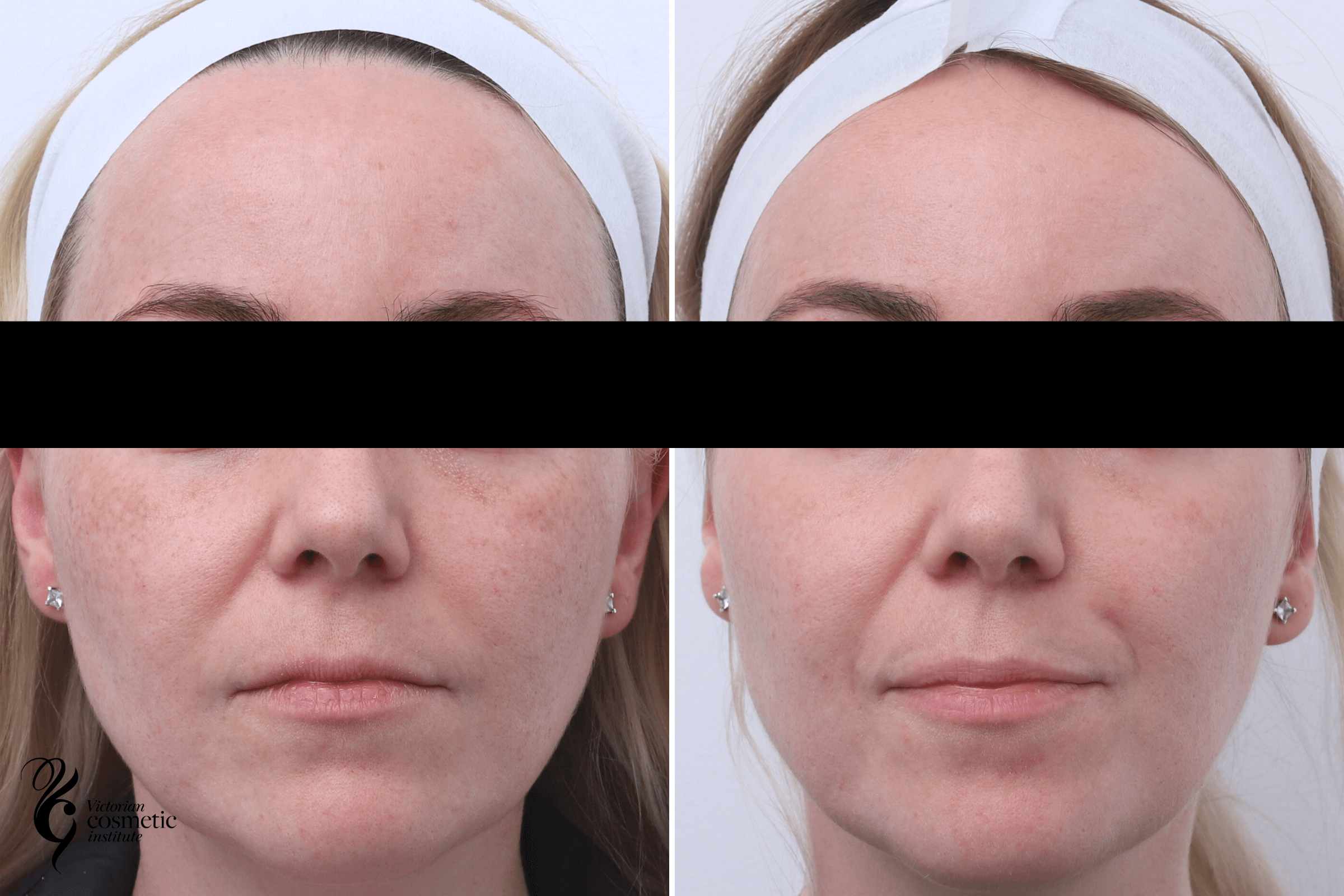
How to treat melasma
It is important to note that melasma is a chronic skin condition, and cannot be cured. However, there are several ways to treat melasma, depending on the type of melasma you have and your skin tone. This includes using lasers to treat melasma and pigmentation. At Victorian Cosmetic Institute we generally use a combination of prescription topical lightening agents, laser treatments, prescription oral medication and at home skin care to lessen the appearance of melasma.
The skin condition also has a strong tendency to return, so maintenance treatments are recommended.
Piqo4 laser
The Piqo4 laser can help reduce melasma over 6-8 sessions conducted weekly or monthly, namely by targeting areas with higher pigmentation with the laser treatment.
Piqo4 laser wavelengths are naturally more attracted to melasma or areas of higher pigmentation than normal skin with less pigmentation. The light is applied to affected areas through very short picosecond pulses (as short as a few trillionths of a second) that help to shatter the melasma pigmentation.
These very short pulses deliver minimal heat energy to the skin and therefore have more of a mechanical effect on the pigmentation rather than a heating effect on the pigmentation. This mechanical effect allows the breakdown of pigmentation without heating the skin and worsening the pigmentation.
The downtime for Piqo4 laser treatment is minimal, with only mild redness lingering on the targeted skin for a day. There are no restrictions on what you can and cannot do after this melasma treatment has occurred.
Fraxel laser
The Fraxel laser is another laser option for the treatment of melasma. As the name suggests, the Fraxel laser only treats a fraction of the skin, firing micro-columns of laser energy into the areas with higher levels of pigmentation. The fractional nature of the laser allows the melasma pigmentation to break down and extrude from the skin.
This particular melasma treatment has the benefit of two wavelengths that penetrate different depths within the skin, targeting melasma at all levels. Usually, 2-3 treatments are required, and there may be a few days of recovery required post-treatment to let the redness and swelling subside.
IPL
Another laser treatment known as IPL can also be used in treating melasma. The pulses of light energy emitted by the laser treatment are absorbed by pigmented cells in the skin, which causes them to break down and naturally be removed by the body’s healing process over time.
The wavelength of the light is adjusted to address your skin condition specifically, but aftercare is still very necessary afterwards. Including that exercise is to be avoided for 1-2 days, while excessive sun exposure and exfoliation should be removed from your daily activities for at least a week.
IPL is a great maintenance option post a course of laser treatments, or as a stand alone treatment for mild melasma cases.
Chemical peels
Chemical peels can help speed the process of improvement from melasma by helping with skin turnover, while also shifting the melanin deposits from the affected area. Usually, a light chemical peel is used, as stronger chemical peels can often stimulate new pigmentation production.
How to manage melasma at home
There are measures you can implement at home to help manage the appearance of melasma pigmentation.
Sunscreen
Using sunscreen daily, irrespective of the weather or your planned (or unplanned) exposure to the sun, is very important. Daily application can protect your skin from damaging UV rays, which may prevent the onset of melasma. Broad-spectrum sunscreen is the most ideal choice to apply on the face and body.
Topical lightening agents
Topical lightening agents may help significantly lighten melasma, as well as prevent it from spreading, especially when used in conjunction with daily sunscreen.
While pigmentation skincare products with lightening agents can reduce the appearance of melasma in the skin, other specific ingredients within medical grade skincare, can also be used to help in the treatment of melasma, including:
- Vitamin C: Vitamin C is commonly used for treating epidermal melasma, as the topical application can not only protect the skin from UV rays, but also target melasma pockets. Products like vitamin C serums can be used to brighten your complexion and skin tone.
- Kojic acid: Kojic acid acts as a tyrosinase inhibitor, preventing the production of melanin.
- Hydroquinone: Especially useful for epidermal melasma, this compound can help break down the overproduction of melanin in the skin.
- Azelaic acid: A naturally occurring acid that also inhibits tyrosinase, but mainly operates to reduce free radical production in the skin that can cause melasma.
- Retinoids: An ingredient commonly seen in retinol serums and vitamin A skin care may help interrupt the melanin process and remove built-up pigmentation.
- Glycolic acid: When combined with other agents in a product, this acid directly reduces melanin formation which leads to pigmentation.
If you see these ingredients in brightening serums or pigmentation serums, they may successfully target hyperpigmented areas and reduce the appearance of brown spots.
Oral medication
There are severe oral medications that can be used to treat melasma, like oral tranexamic acid. Traditionally, it has been used to stop bleeding, particularly during menstruation or post-dental extraction, but in smaller doses can be used to prevent the formation of melanin in response to UV radiation.
Who is a suitable candidate for melasma treatment?
A consultation with one of our practitioners can help determine whether you are a suitable candidate for melasma treatment.
Who is not a suitable candidate for melasma treatment?
You may not be a suitable candidate for melasma treatment if you have:
- A history of, or current infection of cold sores
- A history of keloid scarring
- A diagnosis of HIV/AIDS or immunosuppression
- Current dosages of oral isotretinoin or roaccutane
- Recently had face or brow lift
- A pregnancy or is currently breastfeeding
- A history of severe eczema, seizures or active infections
What are the risks and side effects associated with melasma treatment?
Each melasma treatment comes with its risks and side effects, which will be discussed with your practitioner before treatment begins. They will outline any potential risks that the treatment may pose, as well as provide after-care instructions to deal with any side effects that arise.
FAQs
Can melasma be removed permanently?
Most cases of melasma will fade away with time and treatment, particularly if you take care of your skin and protect it from the sun. Maintenance is required to prolong results from your initial course of treatment.
What is the difference between melasma and pigmentation?
The difference between melasma and pigmentation is the cause of the change in skin tones. Although pigmentation is sun-related, melasma often finds its cause as hormonal changes within the body, with the sun exacerbating the symptoms.
How to treat melasma on the face?
With the face being one of the areas most susceptible to pigmentation, there are several treatment options available. At-home remedies like topical lightening agents or oral medication can certainly reduce the signs of skin pigmentation. However, seeking professional help can allow for greater and long-lasting improvements.
Consultation with a practitioner can confirm the best course of action for your skin, and they can provide a proper treatment regimen to follow after your first session. By following the initial treatment with maintenance therapy, you can maintain your skin.
Why choose Victorian Cosmetic Institute as your provider of melasma treatments?
Melasma is a difficult condition to treat, and treated improperly, can often be made worse. At the Victorian Cosmetic Institute, we treat pigmentation concerns such as melasma. We have a wide range of services on offer, including prescription lightening creams, lasers and chemical peels.
Making that first phone call about any cosmetic procedure can be a confronting task, so we have an online enquiry form you can comfortably fill out. Simply book online, otherwise, you can phone us directly on 1300 863 824.